Over time, dreams appear to help take the emotional charge out of challenging memories while enabling us to retain the information we need to make more adaptive decisions in the future. Engaging with dreams can augment and strengthen this process.
By Dr. Leslie Ellis
Paying attention to dreams adds richness, creativity and depth to inner process. Bringing experiential dreamwork into clinical practice also increases the likelihood that clients will experience deep and lasting change. In my recently-published book, A Clinician’s Guide to Dream Therapy (Routledge, 2020), I offer many reasons for therapists to engage in dreamwork, both for themselves, and with clients. I close the book with a chapter on how neuroscience and dreamwork can combine to bring about transformation of core emotional patterns and beliefs. In this article, I offer a summary of these highlights from my book.
Why work with dreams?
“Clinicians who do not pay attention to their clients’ dreams are missing an opportunity to add a compelling dimension of depth, meaning and emotional authenticity to the therapy process. Because dreams often speak the language of metaphor, even the most seemingly-mundane content may carry important meaning that is outside of the dreamer’s immediate awareness. For example, a client who regularly brings dreams to therapy told me in one session that she had lots of dreams the previous night, but nothing important. Her dogs were in the dream, doing what they always do: the younger one pestering the older one who was, in the dream, getting to the point where she simply couldn’t take it anymore and was ready to snap. While acknowledging the dream snippet was literally true, the simple query: “Is there anything in your life like that, anything that you are completely fed up with?” opened up a whole avenue of process for her that was aptly represented by the dogs and may well have been left unexplored had she not mentioned her dream.
In addition to turning our attention to deeper matters, the benefits of working with dreams in clinical practice include the fact that dreams are creative and engage clients in the therapy process. They point to our most salient emotional concerns. They bypass our internal editing process and normal defenses, and so are unflinchingly honest representations of our life situation. Dreams can bring a new and wider perspective on a situation that seems otherwise stuck. They provide diagnostic information and can be indicators of clinical progress. They help to regulate our emotions, and working directly with the feelings dreams engender may strengthen this positive effect. They can be a safe pathway to working with trauma. The ‘big’ dreams we occasionally experience can literally change our lives, and dream therapy can facilitate and integrate this transformation.
Much of what we know about how clinicians use dreams in their practice is captured in a handful of studies that were reviewed by Pesant and Zadra (2004) with the goal of making clinicians aware that integrating dream work into their practice is both beneficial and accessible. The researchers found that while most therapists do work with dreams at least occasionally in their practice, the majority are not comfortable doing so because they feel they lack expertise or the necessary specialized training. In fact, it is most often the clients, not the therapists, who initiate dream work. The review also found evidence that dream work helps increase clients’ self-knowledge and insight, and increases their commitment to therapy, which can be a predictor of good therapy outcomes” (from chapter 1, A Clinician’s Guide to Dream Therapy).
Dreamwork informed by neuroscience can lead to transformation
We will now skip ahead to the final chapter which brings much of the preceding information together. I map a process that touches on how dreams are implicated in the updating of our emotional memories. The following is an abbreviated version of the last chapter: Transformation: Applying neuroscience to dreamwork.
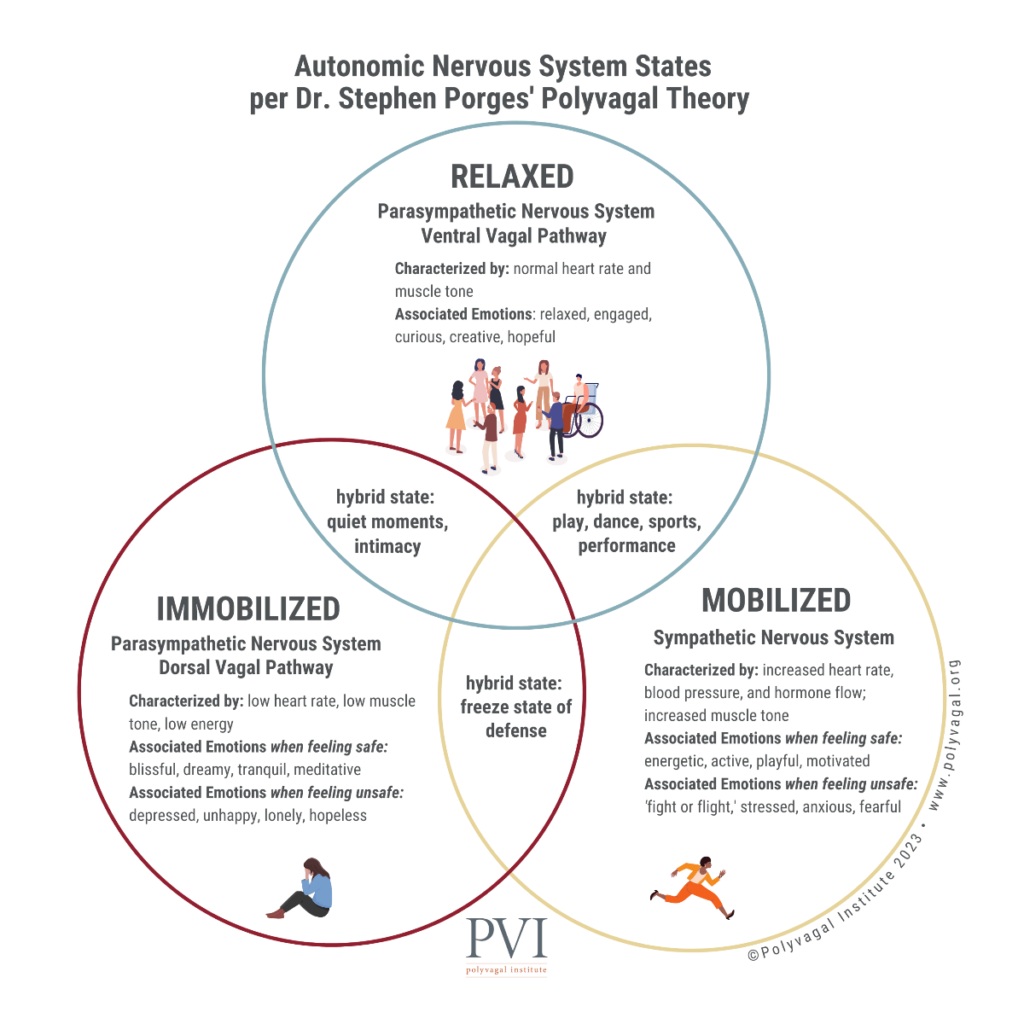
“It used to be thought that emotional memories were not malleable, but the discovery of the processes behind emotional memory reconsolidation (Lane et al., 2015) has changed this view. Current evidence suggests the brain is more resilient and capable of changing and healing than previously thought, even later in life. This is a cause for optimism because now that we know something about the specific mechanisms of change, we can attempt to engineer our therapy processes to engender such changes. The beauty of this kind of change, which can take place in basic neural structures (at the synaptic level), is that once it has taken root, the test of success is that clients maintain the changed behavior automatically and without effort. This is not the white-knuckling kind of change that reverts back to its former patterns under stress.
Implicit emotional patterns are malleable, and can permanently transform into more up-to-date responses, but only under the right circumstances. It used to be thought that long-term emotional memory was indelible because it was stored in synapses, in the basic structures of the brain. But Lee and colleagues (2004) have shown that if certain conditions are met, the synapses will destabilize, making revision of fear memory possible without reinforcing the original memory. According to Ecker, Ticic and Hulley (2012), the keys to unlocking the emotional brain involve clear, repeatable steps that involve juxtaposing a deeply-felt experience of an outdated emotional belief with something that feels true in current life, but opposite. This creates instability in the memory, and if the new experience is reinforced in a timely way, it will not just cover over or compete with the old information, but will actually replace it. Ecker and colleagues state that the resulting change will be transformational, rather than incremental. In my experience, this can be the case, but when beliefs arose in different contexts, transformation may take place over time, with repetitive experience of how the new experience contradicts the older paradigm.
Do not treat the trauma itself, but the beliefs that arise from it
This research highlights something important to keep in mind when working with trauma. The traumatic events themselves are not the important focus. The process, and an open curiosity should be directed to the beliefs that arose out of the traumatic events with the understanding that fear generalizes. For example, people who suffered from chronic neglect in childhood often develop the belief that no one is ever there for them. Feeling deeply into the experience of having even one person consistently show up for them has the potential to shift this long-standing emotional pattern. This is why falling in love can be transformational. Implicit emotional beliefs are not generic, however, but quite specific. They must be experienced in the body rather than speculated about with the mind for the change process to initiate.
Such beliefs and their opposites are often referred to in dreams. Jung was the first to notice this pattern. He found it so pervasive that he developed his theory of dreams as compensation around this idea. Although many early theories about dreams have been successfully challenged, this one persists and is incorporated into many current theories that suggest dreams bring new information and have the potential to transform our long-held emotional beliefs based on current experience. Therefore, dream material can be a rich source of experiential information to use as a base for facilitating memory reconsolidation.
Doing what dreams do, only better
This section describes how we can take a dream and by focusing on it, assist in the very processes that dreams are implicated in – those of emotional memory reconsolidation and emotional regulation. Over time, dreams appear to help take the emotional charge out of challenging memories while enabling us to retain the information we need to make more adaptive decisions in the future. Dreamwork can augment and strengthen this process. And it can kick-start a ‘failed’ dreaming process that is not working as it should, as is the case with recurrent nightmares of those suffering from posttraumatic stress disorder (PTSD).
One of the challenges of trying to engender emotional memory reconsolidation is that it can take quite a bit of detective work to uncover an outdated emotional belief that was formed implicitly. Ideas about the nature of the world are often formed in childhood based on experiences from one’s family of origin, and early beliefs are rarely explicit or called into question. Having no other frame of reference as very young children, we see our environment as simply how the world works, and the beliefs we pick up are a way of adapting to the emotional and relational world we found ourselves in. Dreams, however, can bring our emotional beliefs to life as metaphorical images we experience directly. They often represent novel information that contradicts what we believe. Such images are the keys that can unlock the process of emotional memory reconsolidation, updating and transforming how we respond to life situations in light of current experience.
Those who consistently work with dreams as part of their practice of psychotherapy already have an intuitive understanding of how to work with dreams to bring about therapeutic change. Most invite their clients into a deeply experiential sense of the dream, a critical ingredient in the process. Dreams often have within them contrary elements that can be juxtaposed. Inviting the dreamer to deliberately hold this ‘tension of the opposites’ (Jung) can bring about deep and durable emotional shifts.
In my book’s final chapter, I am suggesting that armed with a basic understanding of the role of dreaming in emotional memory consolidation, we may be able to explore the dreams that clients bring to therapy in a way that facilitates or strengthens the helpful processes that dreams are already a part of. Well-considered current theories suggest that: dreams are implicated in the process of reducing the emotional charge of memories that have current relevance; and dreams play a part in updating our store of memories to include current experience, better preparing us for what’s next. This could also serve as a definition of what happens in psychotherapy. Not just the dreams themselves, but the dreamwork process within therapy can facilitate these emotional and memory updating processes. In addition, nightmare treatment research has shown that by using what we know about dreams in specific and thoughtful ways, we can repair sleep-dream-memory processes that are not working well, helping healthy dreaming to resume.
Clinical examples of transformational dreamwork
What I have noticed about the process of memory reconsolidation is that theories of psychotherapy incorporated its basic elements well before the neuroscience underlying the process was discovered. The trend in dreamwork toward greater experiential practices is an example of how therapists intuit and/or learn by experience to use methods that engender change. In addition, Jung’s notion that dreams are compensatory, and Gendlin’s bias control are two ways dreamwork brings about an experiential juxtaposition that can cause significant shifts in the dreamer’s store of emotional memory.
An example of memory reconsolidation at work is shown in the dreamwork with the Grateful Dead dream earlier in this book. Initially, the dreamer is terrified of being shot by ‘Jack’, the man who in waking life had been abusive and was now aware of where the dreamer worked. In the dreamwork, this fear was juxtaposed by the feelings of safety I encouraged her to sink into very deeply. There were at least two safe places in the dream to draw from: memories of her first love, and also being with a group of like-minded people on the bus who prevent Jack from harming her. In a later part of the session, I ask the dreamer to ‘be’ Jack for a minute, another form of juxtaposition; she feels how hollow and sick he is, before we move on to the part of the dream where she is safe on the bus.
There is a palpable release of tension in the course of working with the dream, and this is sustained, which is the hallmark of a successful memory reconsolidation process. The dreamer reported that prior to the dreamwork, she felt very anxious in general, and especially going to work. After the dreamwork, the fear was no longer present. She said, “I’m not holding the charge anymore.” She could walk into work without her usual worried pausing at the threshold, and this was not a conscious, but an effortless, automatic action reflective of a structural change in the nature of her fear memories. Interestingly, in her subsequent dream, she confronts Jack and he apologizes, which is further evidence of change. I believe such dream changes are significant and authentic reflections of clinical change because they happen without conscious volition. The dreamwork also shifted the way the dreamer holds the memories about Jack, with more of a focus on her friends coming to her rescue and her desire to cultivate community in her life.
The ‘new was’
In the preceding example, the client arrives at a new vantage point. From there, she views the past differently, but also, paradoxically, with a sense that it has always been that way. Gendlin (1984), called this the “new was.” He viewed feelings, thinking, actions and words all primarily as lived experience in the body, and each bodily event as implying what comes next. He called this ‘carrying forward’ and said, “In therapy we change not into something else, but into more truly ourselves. Therapeutic change is into what that person really ‘was’ all along… it is a second past, read retroactively from now. It is a new ‘was’ made from now.” From this new was, steps come that change one’s conception of the past entirely. The change is not just a current one, but a shift that ripples through our entire store of memory, revising many things accordingly.
There is room here to think about state-dependent memory, something I encounter frequently in working as a psychotherapist. To play with the above example, when the client feels afraid, the memories of Jack feel much more ominous and she recalls the worst ones. When she is less afraid, she may recall better times, such as her earlier relationship with her first love. This fear bias colors her perception of the world in general, and of relationships specifically. I believe that the elements of this dream were particularly salient and powerful tools for engendering lasting change in her sense of relational safety. It can be a challenge in psychotherapy to create deeply-felt juxtapositions necessary to revise emotional memory, but dreams provide ready-made and highly relevant material for this powerful transformation process.
Dr. Leslie Ellis is an author, teacher, researcher and therapist with an abiding interest in inner life. She teaches therapists how to work with embodied experience, trauma and dreams, and offers on-line courses in dreamwork and focusing. She has a PhD in Clinical Psychology with a somatic specialization. Shen has conducted award-winning research in treating nightmares of refugees using embodied dreamwork techniques. For more information, go to https://www.drleslieellis.com or contact her at le****@***********is.com.
References
Ecker, B., Ticic, R. & Hulley, L. (2012). Unlocking the emotional brain: Eliminating symptoms at their roots using memory reconsolidation. New York: Routledge.
Ellis, L. (2019). A Clinician’s Guide to Dream Therapy: Implementing Simple and Effective Dreamwork. New York & London: Routledge.
Gendlin, E. T. (1984). The client’s client: The edge of awareness. In R. L. Levant & J. M. Shlien (Eds.), Client-centered therapy and the person-centered approach. New directions in theory, research and practice, pp. 76-107. New York: Praeger.
Lane, R. D., Ryan, L., Nadel, L., & Greenberg, L. (2015). Memory reconsolidation, emotional arousal, and the process of change in psychotherapy. Behavioral and Brain Sciences, 38.
Lee, J. L., Everitt, B. J., & Thomas, K. L. (2004). Independent cellular processes for hippocampal memory consolidation and reconsolidation. Science, 304, 839-843.
Pesant, N. & Zadra, A. (2004). Working with dreams in therapy: What do we know and what should we do? Clinical Psychology Review, 24, 489–512.