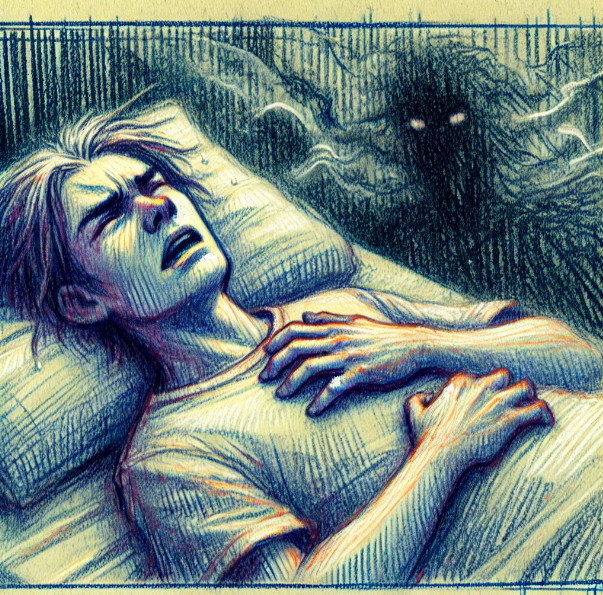
John’s nightmares visit often, and when they wake him up, he can feel his heart racing and his palms sweating. He has been putting off therapy to address the trauma he knows is fueling his nightmares because it’s just so hard face it. What he doesn’t realize is that this avoidance not only disrupts his peace of mind, but also puts him at higher risk for a heart attack or stroke.
It’s well-known that nightmares can disrupt sleep and affect daytime mood, and that they are associated with a wide range of mental health diagnoses, including post-traumatic stress and increased risk of suicide. What is more recently becoming clear is that nightmares are bad for physical health as well — specifically an increased risk of cardiovascular disease. While I have long been advocating for increased awareness and treatment of nightmares, heart health is yet another reason to pay attention to nightmares. This post summarizes some of the key findings on the intricate relationship between cardiovascular health and nightmares from the past five years.
Nightmares and Increased Cardiovascular Risk
Several studies have shown that frequent nightmares are associated with an increased risk of cardiovascular problems. For instance Nadorff and colleagues (2020) found that those who experience persistent nightmares have a higher likelihood of developing cardiovascular disease. This study involved a large cohort of over 3,000 participants and utilized self-reported questionnaires to assess the frequency and intensity of nightmares, as well as the incidence of cardiovascular events. The key finding was that those with frequent nightmares had a significantly higher risk of experiencing cardiovascular events, such as heart attacks and strokes. The study suggests that the stress and anxiety associated with nightmares can lead to increased sympathetic nervous system activity, which, in turn, negatively affects heart health.
Heart Rate Variability (HRV) and Nightmares
HRV, a measure of autonomic nervous system function and cardiac health, has been a focal point in understanding the link between nightmares and cardiovascular health. A study by de Zambotti et al. (2021) included 200 participants and indicated that lower HRV is often observed in individuals with frequent nightmares. Participants underwent polysomnographic sleep studies along with HRV monitoring. The researchers found that decreased HRV, reflecting reduced parasympathetic activity and increased sympathetic dominance, is associated with poor sleep quality and higher nightmare frequency. This imbalance in autonomic function is a potential pathway through which nightmares contribute to cardiac stress and disease.
Nightmares, Sleep Apnea, and Cardiac Stress
Sleep apnea, a condition often co-occurring with nightmares, has also been linked to increased cardiac stress. A study by Basta et al. (2021) involved 150 patients diagnosed with obstructive sleep apnea (OSA) and examined the presence of frequent nightmares. The research utilized polysomnography to monitor sleep and assessed cardiac stress markers such as blood pressure and heart rate. The study showed that patients with both OSA and frequent nightmares exhibited significantly higher levels of cardiac stress markers compared to those without nightmares. The researchers suggest that the intermittent hypoxia and fragmented sleep characteristic of OSA, compounded by the psychological stress of nightmares, can exacerbate cardiovascular strain.
Psychological Stress, Nightmares, and Heart Health
Psychological factors play a crucial role in the relationship between nightmares and heart health. An analysis by Li et al. (2022) reviewed the interplay between psychological stress, nightmare frequency, and cardiovascular outcomes. This review included data from multiple studies, covering a combined participant pool of over 5,000 individuals. The review concluded that the chronic stress response induced by frequent nightmares can lead to hypertension and other cardiovascular issues. The persistent arousal and anxiety from nightmares activate the hypothalamic-pituitary-adrenal (HPA) axis, leading to prolonged cardiovascular strain. These findings were derived from a meta-analysis that consolidated results from various studies, providing a robust understanding of the link between psychological stress from nightmares and cardiovascular health.
Prospective Studies and Longitudinal Data
Longitudinal studies have provided further evidence of the impact of nightmares on long-term cardiac health. A notable study by Ohayon et al. (2021) followed a cohort of 4,500 individuals over ten years. Participants were regularly assessed for nightmare frequency, sleep quality, and cardiovascular health through clinical examinations and self-reported surveys. The study found that those with chronic nightmares had a significantly higher incidence of cardiac events, including heart attacks and strokes, compared to those without frequent nightmares. This study emphasizes the potential long-term cardiovascular risks associated with untreated sleep disturbances like nightmares.
Taken together, these recent studies underscore a significant link between nightmares and cardiac health, strongly supporting the notion that frequent nightmares can be a risk factor for heart disease. This relationship is mediated by mechanisms that include increased sympathetic nervous system activity, reduced HRV, and heightened psychological stress. Beyond the well-understood need to reduce stress to promote heart health, directly addressing nightmares using established dream therapy methods has the potential to mitigate some of these risks.
Join me on substack for an ongoing journey into the world of dreaming!
www.https://dreamsdemystified.substack.com/
Subscribe to get full access to my complete book chapters, publication archives, and to come: recordings, lectures, papers and more.
References
Basta, M., Lin, H. M., Peppard, P. E., & Young, T. (2021). Cardiovascular disease prevalence in patients with obstructive sleep apnea and frequent nightmares. Journal of Clinical Sleep Medicine, 17(1), 17-23. https://doi.org/10.5664/jcsm.8616
de Zambotti, M., Goldstone, A., Colrain, I. M., & Baker, F. C. (2021). Cardiac autonomic regulation during sleep and the relation with nightmares in women with PTSD. Psychosomatic Medicine, 83(3), 299-306. https://doi.org/10.1097/PSY.0000000000000895
Li, S. X., Lam, S. P., Yu, M. W., & Wing, Y. K. (2022). Nightmares and cardiovascular health: A review of recent evidence. Sleep Medicine Reviews, 58, 101453. https://doi.org/10.1016/j.smrv.2021.101453
Nadorff, M. R., Liu, X., & Germain, A. (2020). Nightmares and cardiovascular health: A longitudinal study. Sleep, 43(5), zsz247. https://doi.org/10.1093/sleep/zsz247
Ohayon, M. M., Carskadon, M. A., Guilleminault, C., & Vitiello, M. V. (2021). Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep, 44(5), zsab012. https://doi.org/10.1093/sleep/zsab012