A brief review of Trauma and the Soul: A psycho-spiritual approach to human development and its interruption by Donald Kalsched (Routledge, 2013)
In his book Trauma and the Soul, Kalsched (2013) asks us to stand between two worlds – with our embodied sense of all the trauma that is present in ourselves and in the world, but also with the richness that is our personal, immediate and infinite current existence. He poses the question, “How do we manage to live a full life between these two worlds?” (p. 2).
Kalsched believes that any complete view of the personal self “must include its infinite reach and spiritual potential as well as its finite limitations.” In fact, in working with the deep ravages of complex trauma, it is the depth of connection with one’s soul that is often the saving grace and the “ultimate source of transformation in psychotherapy.”
He notes that many of those who experienced early childhood trauma describe “a blurring of the boundaries between ordinary and non-ordinary reality… that is inaccessible to better adapted people” (p. 3). But one of Kalsched’s primary messages is that these inner protectors from the spirit realm often turn into inner persecutors. How to overcome this phenomenon, not often talked about, is the focus of Trauma and the Soul.
The archetypal world is there to catch trauma survivors when they fall
It is well understood that when a difficult situation exceeds a person’s ability to cope with it, they split off a part of themselves as a form of protection, and in doing so, often step into a vast transpersonal world. Dissociation drops the trauma survivor into a mysterious world that Kalsched argues is not simply the result of ‘splitting’ but is also a doorway into an archetypal world that is “already there to catch them” (p. 4).
To view these extraordinary experiences as metaphor for personal experience collapses the two worlds… “between which our lives are normally suspended.” To assume it is all bounded by personal experience is to lose something essential, and in the case of survivors of extreme trauma, to discount their personal experience as merely imagination. This does not mean that we should overvalue the magical world many trauma survivors inhabit as they often need to be “talked down from their celestial scaffolding… and reconnected to life.” But Kalsched stresses that “often the early story of the trauma survivor is a mythological story before it is a personal one.”
What current neuroscience of infancy shows is that dissociation due to trauma or neglect will fragment experience, storing it in implicit memory only. Kalsched suggests these fragments gather up archetypal images from the collective unconscious because there has not yet been a developmental step that differentiates into a personal self. So early trauma survivors find access to and expression of their story more easily through myth, dreams and metaphor.
The body is the access point for this material, and focusing remains one of the best ways I know to gain access to this metaphysical layer. Focusing is an inner process that gently opens a person up to their embodied, implicit knowledge. The process of accessing, and expressing what a trauma survivor embodies can move the material from the transpersonal to be woven into their personal story. To pathologize this process and label it as a form of psychosis is unhelpful, possibly harmful – though the ultimate goal is to enable the client to straddle both worlds while remaining in solid contact with what is real and present… at times a tricky balancing act.
Kalsched makes a careful distinction here. He states that “the spiritual world is real, and following trauma it is recruited for defensive purposes” (p. 5). He believe that the angels and demons that help or haunt survivors are not only the derivatives of a defensive process, something that would not exist otherwise.
In viewing the archetypal realm as its own form of reality, Kalsched does not dismiss the visible world or the importance of our new understanding of the role of attachment and early relationship. He said these developments keep trauma work “relevant and grounded. In fact, they even hold out the possibility of restoring the embodied soul to our field” (p. 8). I suspect the reason he devotes more attention to the invisible world is that it is too often ignored, and in trauma work, this is an oversight. He writes that the infinite and eternal world of spirit “is often potentiated by early trauma and so a complete story of trauma must include its perspective.”
Trauma is defined as anything we are unable to bear consciously. Children are especially vulnerable because they have not yet developed any way to metabolize abuse or neglect, and so their nascent sense of self would be shattered if it were not for our ability to split or dissociate to “save a part of the child’s innocence and aliveness, preserving it in the unconscious… and surrounding it with an implicit narrative that is eventually made explicit in dreams” (p. 11).
Newfound hope that healing is possible
Kalsched found that such dreams contained a pattern, a dyad of child or animal and its protector, often a diabolical figure that would appear just as the client was making progress in therapy – getting close enough to relational feelings to trigger a defensive response. In 1996, Kalsched wrote about this ‘self-care’ system without much hope, but he has since incorporated techniques informed by attachment and neuroscience (ie Schore, Badenoch, Bromberg). “As a result, I have been able to witness how the seemingly-intractable resistances of the self-care system can transform, and the defensive system can even release its prisoners” (p. 13). This work is not easy and involves the full relational participation of the therapist to bring about “the co-creation of an entirely new inter-subjective reality.”
Kalsched was fascinated with what is preserved when a traumatized child splits off and hides away an essential part of themselves. He originally called it the “imperishable personal spirit” and now calls it simply the soul. He called the “main epiphany” of Jung’s work the discovery of “the divine child, patiently awaiting his conscious realization” (1912, para 510). Kalsched points out that there is a sacred dimension we can discern from “the psyche’s symbolic process – if we learn how to attend to it in our dreams” (p. 15).
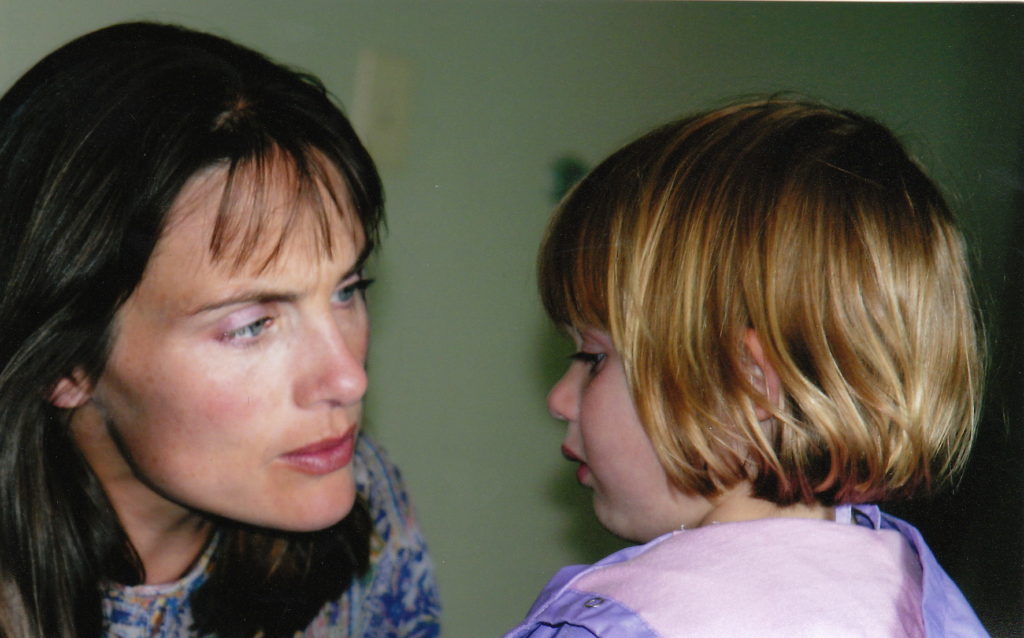
Kalsched echoes the popular sentiment that early trauma is relational trauma and this can only be healed in relationship. He stresses that such a healing relationship must be of a particular kind that looks both outward and inward. It can bridge dissociated self-states in a manner not unlike the ‘good-enough’ infant-mother dyad made famous by Winnicott. It can weather “the stormy affects that are generated as the soul re-enters the body, until re-connections are made between affect and images, between the present and the past, between the inner child and its caretakers. Such a relationship holds the hope that both inner and outer transitional space may open once again, that connections in the brain can slowly be re-wired, and that archetypal defenses will release us into human inter-subjectivity and ensouled living” (p. 21).
He adds that “therapy for the soul comes in many forms” in addition to therapy or parent-child relationship, including encounters with animals, art, ideas, music… there is no formula or system that applies universally. “This theory can never be systematic or scientific because the soul and spirit are mercurial realities, quixotic, ineffable and can never be pinned down… If we were wise, we would probably keep silent about the soul and learn to listen” (p. 22).